General Conditions
Erectile Dysfunction (ED)
What is Erectile Dysfunction?
Erectile dysfunction, or ED, is the most common sex problem that men report to their doctor. It affects as many as 30 million men.
ED is defined as trouble getting or keeping an erection that’s firm enough for sex.
Though it’s not rare for a man to have some problems with erections from time to time, ED that is progressive or happens routinely with sex is not normal, and it should be treated.
ED can happen:
- Most often when blood flow in the penis is limited or nerves are harmed
- With stress or emotional reasons
- As an early warning of a more serious illness, like: atherosclerosis (hardening or blocked arteries), heart disease, high blood pressure or high blood sugar from Diabetes
Finding the cause(s) of your ED will help treat the problem and help with your overall well-being. As a rule, what’s good for your heart health is good for your sex health.
How Erections Work
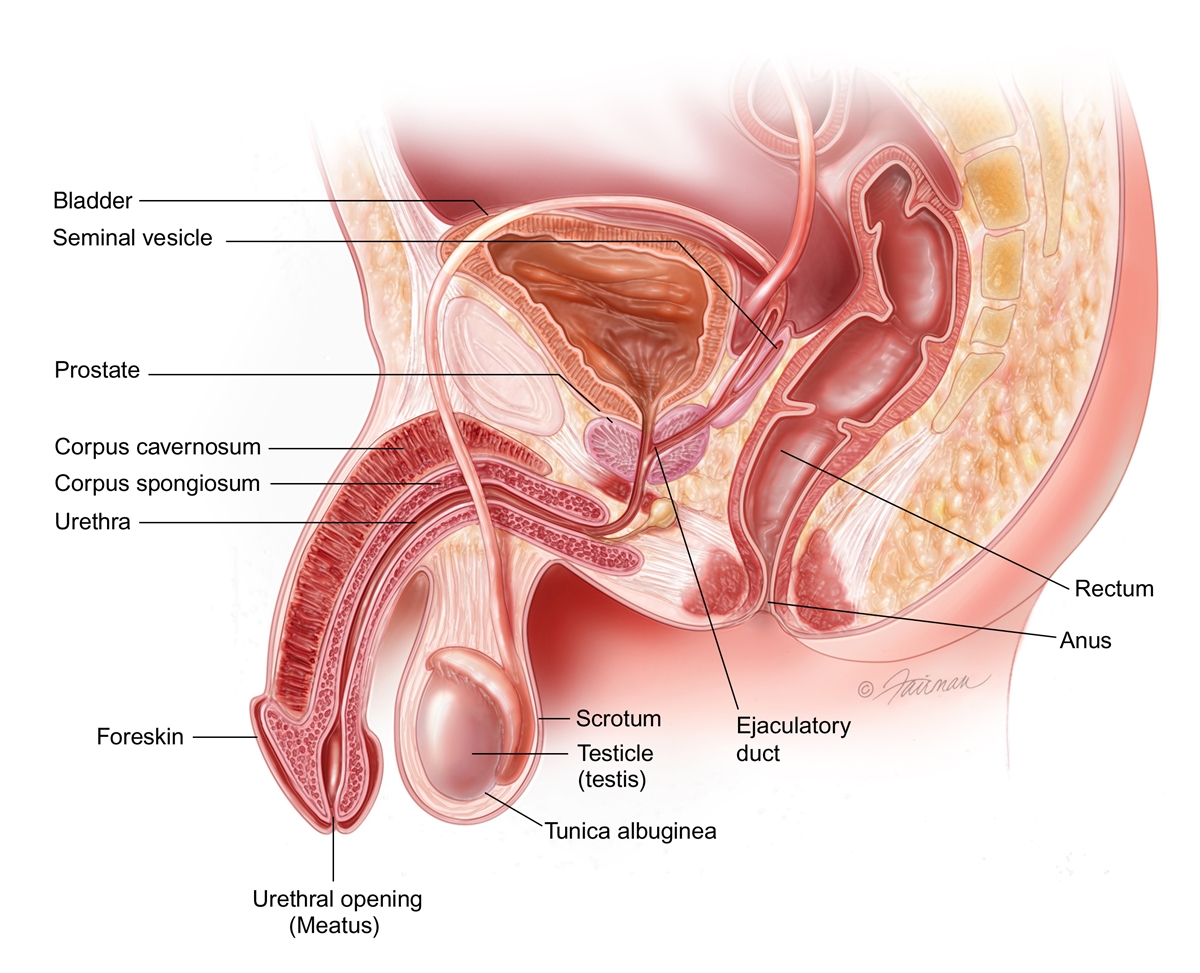
During sexual arousal, nerves release chemicals that increase blood flow into the penis. Blood flows into two erection chambers in the penis, made of spongy muscle tissue (the corpus cavernosum). The corpus cavernosum chambers are not hollow.
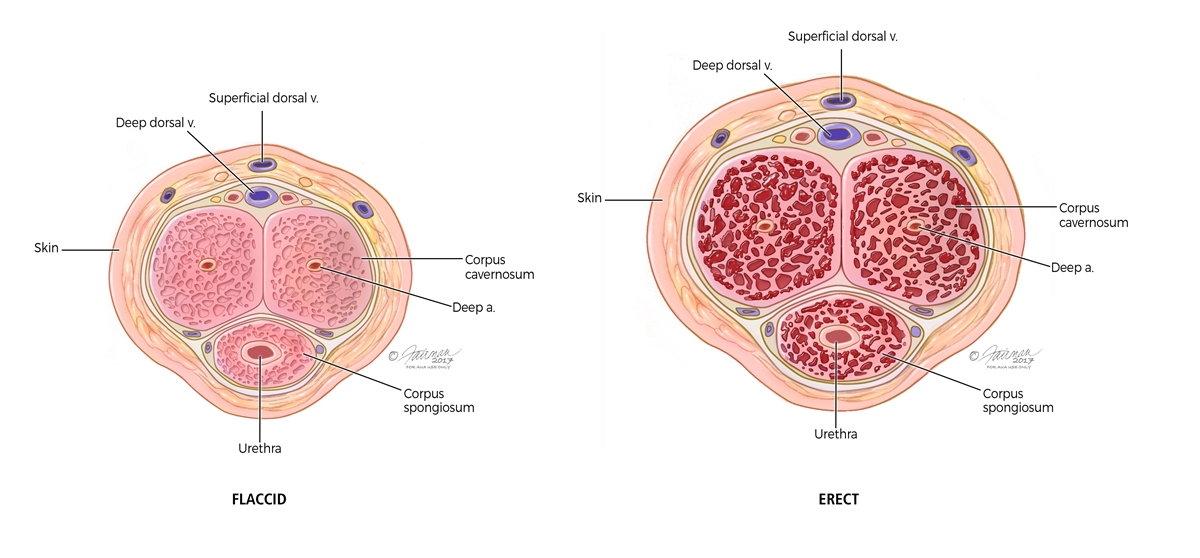
During erection, the spongy tissues relax and trap blood. The blood pressure in the chambers makes the penis firm, causing an erection. When a man has an orgasm, a second set of nerve signals reach the penis and cause the muscular tissues in the penis to contract and blood is released back into a man’s circulation and the erection comes down.
When you are not sexually aroused, the penis is soft and limp. Men may notice that the size of the penis varies with warmth, cold or worry; this is normal and reflects the balance of blood coming into and leaving the penis.
Procedures
- Urowave therapy: Urowave therapy is a non-invasive treatment for erectile dysfunction (ED) that uses low-intensity shock waves to enhance blood flow and promote tissue regeneration, offering a long-term solution for many men. Urowave therapy, also known as low-intensity extracorporeal shock wave therapy (Li-ESWT), is a treatment designed to address erectile dysfunction by using sound waves to stimulate blood flow in the penis. This therapy aims to regenerate erectile tissue, improve blood vessel formation, and enhance overall erectile function.
Treatment Sessions: Typically, patients undergo a series of six sessions, each lasting about 15 minutes. The treatment is painless and does not require anesthesia.
Insurance Coverage: It’s important to note that while initial consultations may be covered by insurance, the Urowave treatment itself typically is not.
- Penile implant procedure: Is a surgical treatment for erectile dysfunction when other therapies—such as medications, injections, or vacuum devices—have been ineffective or are not appropriate. During the procedure, a urologist surgically places a medical device inside the penis that allows a man to achieve an erection suitable for sexual activity. The implant does not affect sensation, orgasm, or ejaculation.
There are two main types of penile implants:
Inflatable penile implant
- Consists of two cylinders placed in the penis, a pump placed in the scrotum, and a fluid reservoir placed in the abdomen
- The patient activates the pump to create an erection and deflates it after intercourse
- This is the most commonly used type due to its natural appearance and function
Malleable (semi-rigid) implant
- Consists of bendable rods placed in the penis
- The penis is manually positioned for intercourse
- Simpler device with fewer mechanical parts
The surgery is typically performed under general anesthesia and usually takes 1–2 hours. Most patients go home the same day or after a short hospital stay. Recovery includes a period of healing before the device is activated, usually around 4–6 weeks.
Treatments
Treatment for erectile dysfunction depends on the underlying cause, severity of symptoms, and patient preference. Options range from lifestyle changes to medical therapies.
- Oral Medications (PDE-5 Inhibitors)
Often the first-line treatment.
- Examples: Sildenafil (Viagra®), Tadalafil (Cialis®)
- Improve blood flow to the penis
- Require sexual stimulation to be effective
- Not appropriate for patients taking nitrates or with certain heart conditions
- Lifestyle Modifications
Often recommended alongside medical therapy.
- Weight loss and regular exercise
- Smoking cessation
- Limiting alcohol intake
- Managing diabetes, high blood pressure, and cholesterol
- Vacuum Erection Devices (VED)
- A mechanical pump draws blood into the penis
- A constriction ring helps maintain the erection
- Non-invasive and medication-free
- May cause temporary bruising or discomfort
- Penile Injections (Intracavernosal Injection Therapy)
- Medications such as Trimix are injected directly into the penis
- Highly effective, including in patients who do not respond to oral medications
- Requires patient education and careful dosing
- Hormone Therapy
- Used in patients with confirmed low testosterone levels
- Testosterone replacement may improve erectile function in selected patients
- Not effective if testosterone levels are normal
Incontinence
What is Urinary Incontinence?
Urinary incontinence is leaking of urine that you can’t control. Many American men and women suffer from urinary incontinence. We don’t know for sure exactly how many. That’s because many people do not tell anyone about their symptoms. They may be embarrassed, or they may think nothing can be done. So they suffer in silence.
Urinary incontinence is not just a medical problem. It can affect emotional, psychological and social life. Many people who have urinary incontinence are afraid to do normal daily activities. They don’t want to be too far from a toilet. Urinary incontinence can keep people from enjoying life.
Many people think urinary incontinence is just part of getting older. But it’s not. And it can be managed or treated. Learn more here. Talk to your doctor. Find out what treatment is best for you.
Key Statistics
A quarter to a third of men and women in the U.S. suffer from urinary incontinence. That means millions of Americans. About 33 million have overactive bladder (also known as OAB) representing symptoms of urgency, frequency and with or without urge incontinence.
Studies show that many things increase risk. For example, aging is linked to urinary incontinence. Pregnancy, delivery, and number of children increase the risk in women. Women who have had a baby have higher rates of urinary incontinence. The risk increases with the number of children. This is true for cesarean section (c-section) and vaginal delivery.
Women who develop urinary incontinence while pregnant are more likely to have it afterward. Women after menopause (whose periods have stopped) may develop urinary incontinence. This may be due to the drop in estrogen (the female sex hormone). Taking estrogen, however, has not been shown to help urinary incontinence.
Men who have prostate problems are also at increased risk. Some medications are linked to urinary incontinence and some medicines make it worse. Statistics show that poor overall health also increases risk. Diabetes, stroke, high blood pressure and smoking are also linked.
Obesity increases the risk of urinary incontinence. Losing weight can improve bladder function and lessen urinary incontinence symptoms.
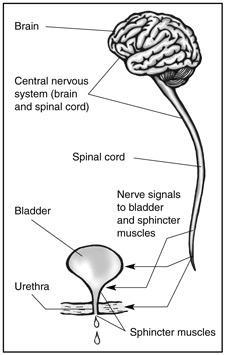
What happens normally?
The brain and the bladder control urinary function. The bladder stores urine until you are ready to empty it. The muscles in the lower part of the pelvis hold the bladder in place. Normally, the smooth muscle of the bladder is relaxed. This holds the urine in the bladder. The neck (end) of the bladder is closed. The sphincter muscles are closed around the urethra. The urethra is the tube that carries urine out of the body. When the sphincter muscles keep the urethra closed, urine doesn’t leak.
Once you are ready to urinate, the brain sends a signal to the bladder. Then the bladder muscles contract. This forces the urine out through the urethra, the tube that carries urine from the body. The sphincters open up when the bladder contracts.
What are the types of urinary incontinence?
Urinary incontinence is not a disease. It is a symptom of many conditions. Causes may differ for men and women. But it is not hereditary. And it is not just a normal part of aging. These are the four types of urinary incontinence:
Stress Urinary Incontinence (SUI)
With SUI, weak pelvic muscles let urine escape. It is one of the most common types of urinary incontinence. It is common in older women. It is less common in men.
SUI happens when the pelvic floor muscles have stretched. Physical activity puts pressure on the bladder. Then the bladder leaks. Leaking my happen with exercise, walking, bending, lifting, or even sneezing and coughing. It can be a few drops of urine to a tablespoon or more. SUI can be mild, moderate or severe.
There are no FDA approved medicines to treat SUI yet, but there are things you can do. Ways to manage SUI include “Kegel” exercises to strengthen the pelvic floor. Lifestyle changes, vaginal and urethral devices, pads, and even surgery are other ways to manage SUI.
Overactive Bladder (OAB)
OAB is another common type of urinary incontinence. It is also called “urgency” incontinence. OAB affects more than 30% of men and 40% of women in the U.S. It affects people’s lives. They may restrict activities. They may fear they will suddenly have to urinate when they aren’t near a bathroom. They may not even be able to get a good night’s sleep. Some people have both SUI and OAB and this is known as mixed incontinence.
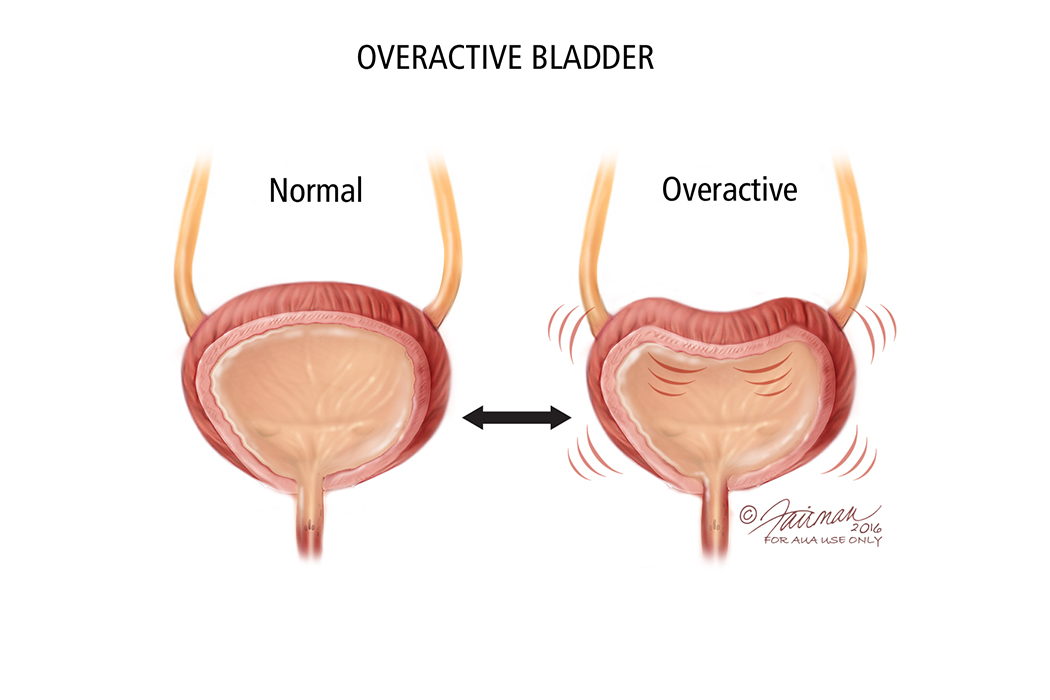
With OAB, your brain tells your bladder to empty – even when it isn’t full. Or the bladder muscles are too active. They contract (squeeze) to pass urine before your bladder is full. This causes the urge (need) to urinate.
The main symptom of OAB is the sudden urge to urinate. You can’t control or ignore this “gotta go” feeling. Another symptom is having to urinate many times during the day and night.
OAB is more likely in men with prostate problems and in women after menopause. It is caused by many things. Even diet can affect OAB. There are a number of treatments. They include life style changes, drugs that relax the bladder muscle, or surgery. Some people have both SUI and OAB.
Mixed Incontinence (SUI and OAB)
Some people leak urine with activity (SUI) and often feel the urge to urinate (OAB). This is mixed incontinence. The person has both SUI and OAB.
Overflow Incontinence
With overflow incontinence, the body makes more urine than the bladder can hold or the bladder is full and cannot empty thereby causing it to leak urine. In addition, there may be something blocking the flow or the bladder muscle may not contract (squeeze) as it should.
One symptom is frequent urinating of a small amount. Another symptom is a constant drip, called “dribbling.”
This type of urinary incontinences is rare in women. It is more common in men who have prostate problems or have had prostate surgery.
Procedures
- Nerve stimulation therapies
- Sacral neuromodulation Axonics and Medtronic Interstim:
- Implanted device (bladder pacemaker)
- High success rates
- Botox injections (intravesical onabotulinum toxin)
- Very effective for refractory urge incontinence
- Lasts ~6–9 months
- Risk: urinary retention, UTIs
- Repeat treatments required
Botox relaxes the bladder muscle and reduces involuntary contractions.
Treatments
First-line (Lifestyle & Behavioral)
These are usually recommended for everyone because they’re safe and effective:
- Bladder training (timed voiding, gradually increasing intervals)
- Pelvic floor exercises (Kegels) ± pelvic floor physical therapy
- Fluid and diet changes
- Reduce caffeine, alcohol, carbonation, artificial sweeteners
- Weight loss if overweight
- Constipation treatment
- Smoking cessation
Behavioral therapies often significantly improve symptoms and may be enough alone for mild cases.
Medications
Used when lifestyle changes aren’t enough.
- Anticholinergics (antimuscarinics)
Relax bladder muscle contractions.
Examples:
- Oxybutynin
- Tolterodine
- Solifenacin
- Darifenacin
- Trospium
- Fesoterodine
Common side effects:
- Dry mouth
- Constipation
- Blurry vision
- Cognitive effects (especially in older adults)
These drugs block acetylcholine signals that trigger bladder contractions.
- Beta-3 agonists
Often preferred now due to fewer side effects.
Examples:
- Mirabegron
- Vibegron
They relax the bladder and increase storage capacity.
- Topical vaginal estrogen (post-menopausal women)
Can improve urinary symptoms by strengthening tissues around the urethra. May help with SUI symptoms also.
Kidney Stones
What are Kidney Stones?
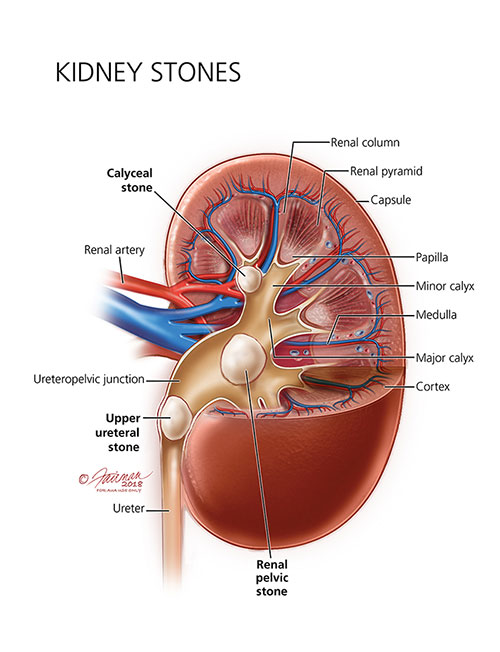
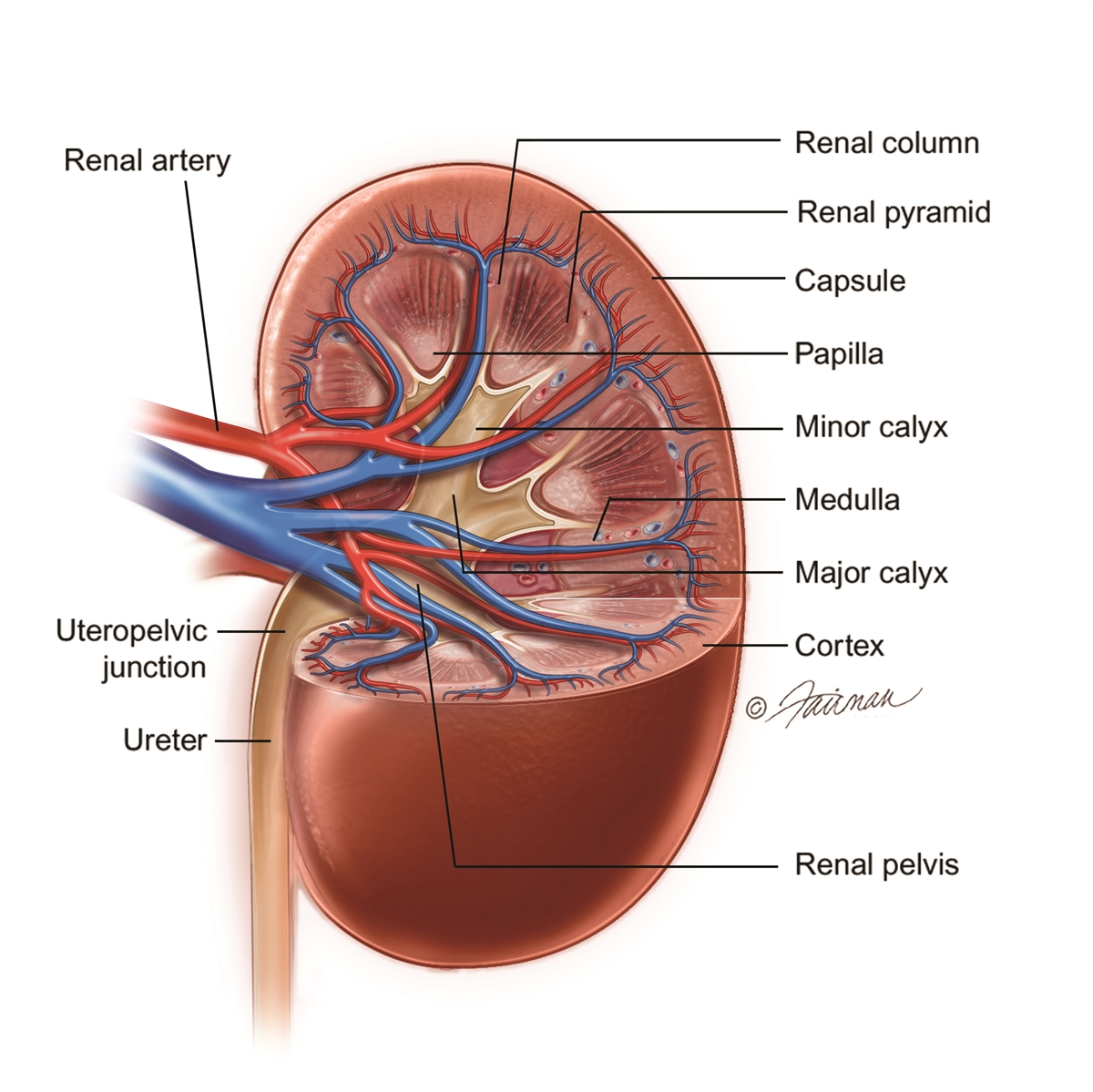
Urine contains many dissolved minerals and salts. When your urine has high levels of these minerals and salts, you can form stones. Kidney stones can start small but can grow larger in size, even filling the inner hollow structures of the kidney. Some stones stay in the kidney, and do not cause any problems. Sometimes, the kidney stone can travel down the ureter, the tube between the kidney and the bladder. If the stone reaches the bladder, it can be passed out of the body in urine. If the stone becomes lodged in the ureter, it blocks the urine flow from that kidney and causes pain.
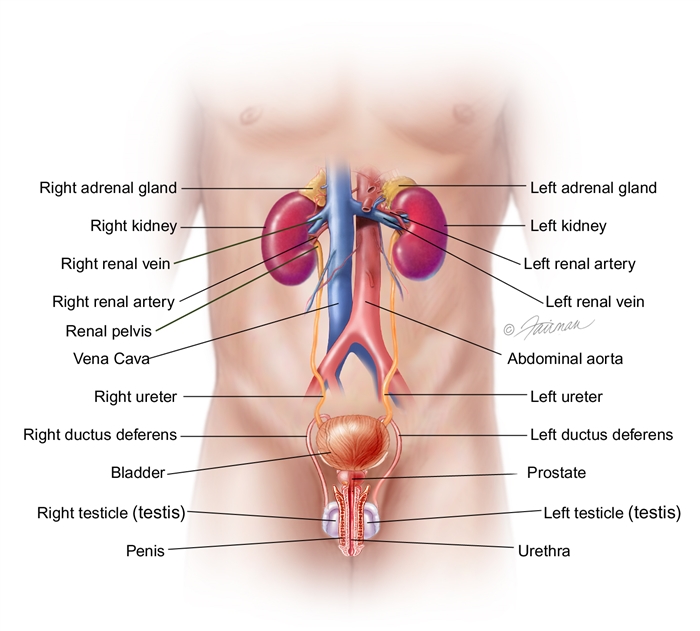
The Kidneys and Urinary System
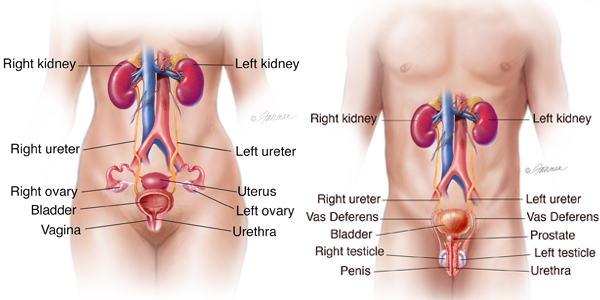
The kidneys are fist-size organs that handle the body’s fluid and chemical levels. Most people have two kidneys, one on each side of the spine behind the liver, stomach, pancreas and intestines. Healthy kidneys clean waste from the blood and remove it in the urine. They control the levels of sodium, potassium and calcium in the blood.
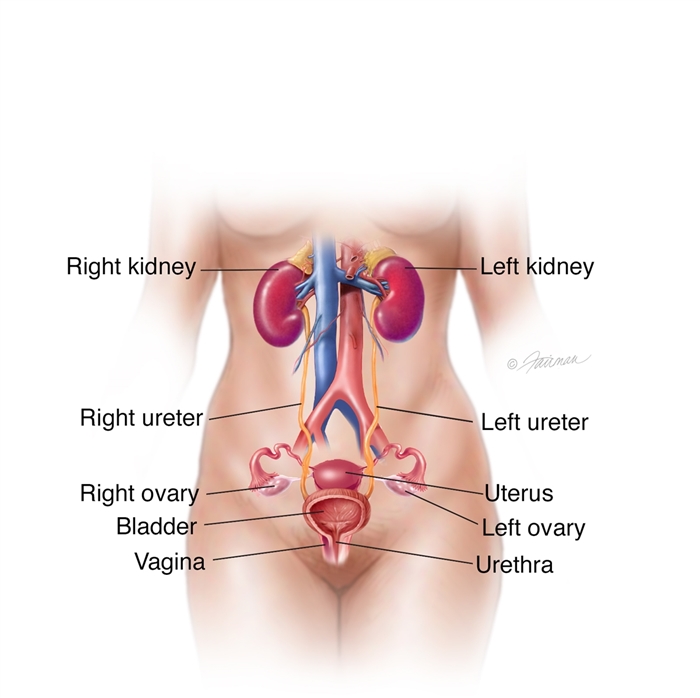
The kidneys, ureters and bladder are part of your urinary tract. The urinary tract makes, transports, and stores urine in the body. The kidneys make urine from water and your body’s waste. The urine then travels down the ureters into the bladder, where it is stored. Urine leaves your body through the urethra.
Kidney stones form in the kidney. Some stones move from the kidney into the ureter. The ureters are tubes leading from the kidneys to the bladder. If a stone leaves the kidney and gets stuck in the ureter, it is called a ureteral stone.
What are Kidney Stones Made of?
Kidney stones come in many different types and colors. How you treat them and stop new stones from forming depends on what type of stone you have.
Calcium stones (80 percent of stones)
Calcium stones are the most common type of kidney stone. There are two types of calcium stones: calcium oxalate and calcium phosphate. Calcium oxalate is by far the most common type of calcium stone. Some people have too much calcium in their urine, raising their risk of calcium stones. Even with normal amounts of calcium in the urine, calcium stones may form for other reasons.
Uric acid stones (5-10 percent of stones)
Uric acid is a waste product that comes from chemical changes in the body. Uric acid crystals do not dissolve well in acidic urine and instead will form a uric acid stone. Having acidic urine may come from:
- Being overweight
- Chronic diarrhea
- Type 2 diabetes (high blood sugar)
- Gout
- A diet that is high in animal protein and low in fruits and vegetables
Struvite/infection stones (10 percent of stones)
Struvite stones are not a common type of stone. These stones are related to chronic urinary tract infections (UTIs). Some bacteria make the urine less acidic and more basic or alkaline. Magnesium ammonium phosphate (struvite) stones form in alkaline urine. These stones are often large, with branches, and they often grow very fast.
People who get chronic UTIs, such as those with long-term tubes in their kidneys or bladders, or people with poor bladder emptying due to neurologic disorders (paralysis, multiple sclerosis, and spina bifida) are at the highest risk for developing these stones.
Cystine stones (less than 1 percent of stones)
Cystine is an amino acid that is in certain foods; it is one of the building blocks of protein. Cystinuria (too much cystine in the urine) is a rare, inherited metabolic disorder. It is when the kidneys do not reabsorb cystine from the urine. When high amounts of cystine are in the urine, it causes stones to form. Cystine stones often start to form in childhood.
Procedures
Conservative (No Procedure)
- Hydration — drinking plenty of fluids to help pass the stone.
- Pain control — NSAIDs or prescription pain medication.
- Medical expulsive therapy — medications (such as tamsulosin) to relax the ureter and help the stone pass.
- Observation — many stones ≤5 mm pass on their own.
Non-invasive / Minimally Invasive
- Shock Wave Lithotripsy (SWL / ESWL)
Uses sound waves from outside the body to break stones into small pieces that pass in urine.
Best for smaller stones (usually <2 cm) in the kidney or upper ureter. - Ureteroscopy with Laser Lithotripsy
A small scope is passed through the urethra and bladder into the ureter or kidney.
A laser breaks the stone, and fragments are removed.
Often used for ureteral stones or kidney stones that SWL may not treat well.
May require temporary stent placement.
- Shock Wave Lithotripsy (SWL / ESWL)
Surgical Procedure
- Percutaneous Nephrolithotomy (PCNL)
A small incision is made in the back to directly access the kidney.
Used for large stones (>2 cm), staghorn stones, or complex cases.
Highest stone-free rate for large stones.
- Percutaneous Nephrolithotomy (PCNL)
Temporary / Emergency Procedures
- Ureteral Stent Placement
A tube placed between the kidney and bladder to relieve obstruction.
Often done for infection with obstruction or severe pain before definitive treatment. - Percutaneous Nephrostomy Tube
A drain placed directly into the kidney through the back.
Used in emergencies (infection with blockage) or when a stent cannot be placed.
- Ureteral Stent Placement
Treatments
Lifestyle & Diet Changes
- Increase fluids — goal is usually enough intake to produce about 2–2.5 liters of urine per day.
- Reduce sodium (salt) — high sodium increases calcium in the urine.
- Normal calcium intake — do not restrict calcium unless instructed; low calcium can increase oxalate absorption.
- Limit high-oxalate foods (for calcium oxalate stones): spinach, nuts, chocolate, tea, beets.
- Increase citrate intake — citrus fruits (especially lemon/lime) can help prevent stones.
- Maintain healthy weight — obesity increases stone risk.
Medications (when indicated)
- Thiazide diuretics — reduce calcium in urine for calcium stones.
- Potassium citrate — decreases urine ph to reduce stone formation.
- Allopurinol — used for uric acid stones or high uric acid levels.
Monitoring
- 24-hour urine collections — identifies risk factors to guide prevention.
- Blood tests — evaluate metabolic causes.
- Follow-up imaging — monitor for new stones.
Peyronie's
What is Peyronie’s Disease?
Peyronie’s disease is where plaques (segments of flat scar tissue) form under the skin of the penis. These plaques can cause the penis to bend or become indented during erections. The plaques can often be felt through the skin and can be painful.
How Does the Penis Normally Work?
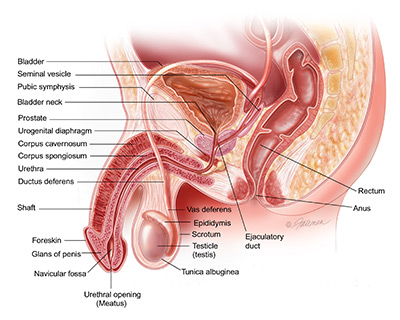
The main roles of the penis are to carry urine and sperm out of the body. There are 3 tubes inside the penis. One is called the urethra. It is hollow and carries urine from the bladder through the penis to the outside. The other 2 tubes are called the corpora cavernosa. These are soft, spongy tubes that fill with blood to make the penis stiff during an erection. The 3 tubes are wrapped together by a very tough fibrous sheath called the tunica albuginea. During sex, the stiffness of the penis makes it hard enough for sex. Then the urethra acts as a channel to carry semen into the vagina.
Symptoms
Peyronie’s disease plaques mostly (70% of the time) form on the top (or dorsal side) of the penis. The plaques make the tunica albuginea less flexible and may cause the penis to bend upwards when it stiffens. When plaques form on the bottom or side of the penis, the bend will be downward or sideways. Some men have more than one plaque, which may cause complex curves.
Sometimes plaques form that go all the way around the penis. These plaques most often do not cause curving but may cause the shaft of the penis to narrow like the neck of a bottle. This is sometimes called “bottle-necking” or “waisting”. In bad cases, the plaque may collect calcium and become very hard, almost like a bone. Men may also notice their penis has shrunk or gotten shorter.
Other signs that you may have Peyronie’s disease are:
- bent/curved penis
- lumps in the penis
- painful erections
- soft erections
- having trouble with sex because of a bent/curved penis
Peyronie’s disease can make your quality of life worse. Over 75 out of 100 men with Peyronie’s disease are stressed and depressed because of it. Unfortunately, many men with Peyronie’s disease are embarrassed and choose to suffer in silence rather than get help.
How Common is Peyronie’s Disease?
Peyronie’s disease is thought to happen in about 4 out of 100 men between the ages of 40 and 70. It is rare in young men but has been seen in men in their 30s. The number of cases may be higher than the estimates because many men may be embarrassed and choose not to see their health care provider.
Interestingly, more Peyronie’s disease cases have been noted in recent years. This may be because new drugs for erectile dysfunction (ED) have come to market and health care providers may notice Peyronie’s disease in men seeking help for ED. For this reason, the number of Peyronie’s disease cases reported may keep growing.
Causes
Peyronie’s disease is likely caused by minor injury to the penis. (See penile trauma.) This type of damage is most often caused by vigorous sex (such as bending the penis during penetration or pressure from a partner’s pubic bone), though it can also be caused by sports or other accidents. Injury to the tunica albuginea may result in scar tissue forming in the cells (fibrosis). This scar tissue then forms the plaque of Peyronie’s disease. Peyronie’s disease is the result of a problem in the way the body heals wounds.
Stages of Peyronie’s
Peyronie’s disease is often split into 2 stages: the acute phase and the chronic phase. During both phases, the bent/curved penis may cause problems with sex. You also may have ED.
Acute Phase: The acute phase usually lasts for 5 to 7 months but can last up to 18 months in rare cases. During this time, the plaques form in the penis, the bending/curving of the penis gets worse and you may feel pain when your penis gets hard.
Chronic Phase: The chronic phase is when the plaque stops growing and the penis doesn’t bend any further. If there was pain with erection during the acute phase, it often will have ended by this time.
Other Factors
Not all men who suffer mild trauma to the penis get Peyronie’s disease. For this reason, most researchers believe there must be genetic or environmental reasons Peyronie’s disease plaques form. Men with certain connective tissue disorders (such as Dupuytren’s contractures or tympanosclerosis) and men who have a close family member with Peyronie’s disease have a greater risk of getting it. Certain health issues, such as high blood sugar, tobacco use, or past pelvic trauma, may also lead to wound healing problems and may help cause Peyronie’s disease.
Procedures
Coming soon…
Treatments
Coming soon…
Prostate Disease (BPH)
What is Benign Prostatic Hyperplasia (BPH)?
Benign prostatic hyperplasia (BPH) is when the prostate and surrounding tissue expands. The prostate goes through two main growth periods as a man ages. The first is early in puberty when the prostate doubles in size. The second begins around age 25 and continues during most of a man’s life. As you age, your prostate may get larger. BPH is when it gets large enough to cause problems.
As the prostate enlarges, it presses against the urethra. The bladder wall becomes thicker. Over time the bladder may weaken and lose the ability to empty fully. Urine then remains in the bladder. These problems cause many of the lower urinary tract symptoms (LUTS) of BPH. How BPH causes symptoms may help your healthcare team determine if and what type of treatment to suggest.
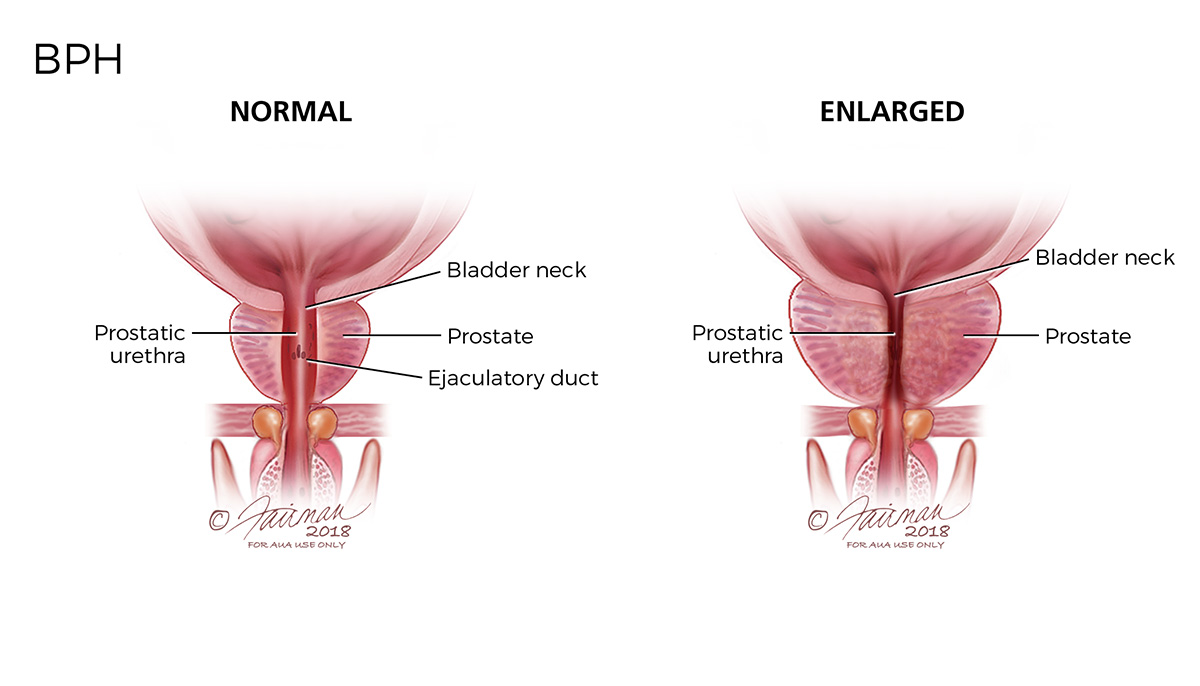
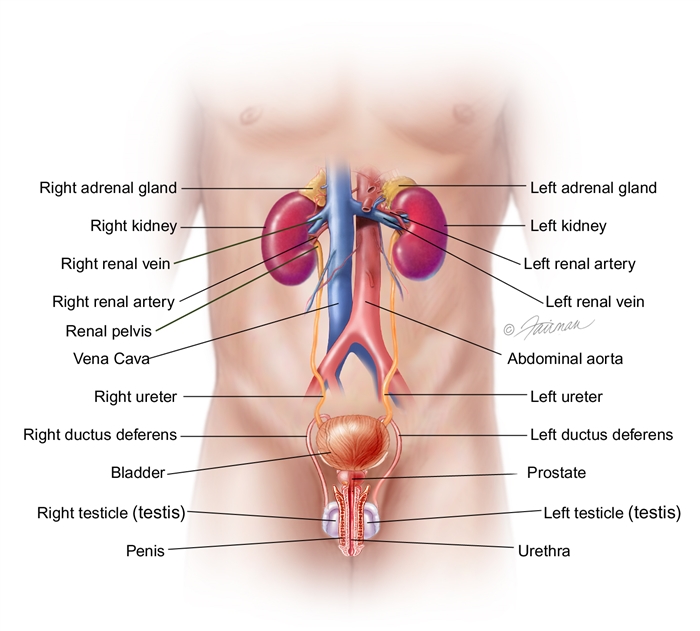
How Does the Prostate Work?
The prostate is part of the male reproductive system. The prostate’s main job is to make fluid for semen. It is about the size of a walnut and weighs an ounce or so. It sits below the bladder and in front of the rectum. It goes around a tube called the urethra. The urethra carries urine from the bladder and out through the penis.
Who is at Risk for BPH?
- Men over the age of 50 as the risk for BPH rises with age
- Men whose fathers had BPH
- Men who are overweight or obese
- Men who don’t stay active
- Some men with erectile dysfunction (ED)
Symptoms
When the prostate is enlarged, it can bother or block the bladder. Needing to pass urine often is a common symptom of BPH. This might include the need to pass urine as often as every one to two hours, mainly at night.
Other symptoms of BPH are listed below:
- Incomplete emptying: the feeling your bladder is full, even after passing urine.
- Frequency: the need to pass urine often, about every one to two hours.
- Intermittency: the need to stop and start several times when passing urine.
- Urgency: feeling the urgent need to pass urine as if you can’t wait.
- Weak stream: a weak urine flow.
- Straining: trouble starting to pass urine or the need to push or strain to pass urine.
- Nocturia: the need to wake up at night more than two times to pass urine.
Causes
The causes of BPH are not clear. It mainly occurs in older men. Hormone changes are thought to play a role.
Hormones from the testis may be the main factor. For example, as men age, the amount of active testosterone in the blood declines. Estrogen levels stay the same. BPH may occur when these hormone changes trigger prostate cell growth. Another theory is about the role of dihydrotestosterone (DHT.) This male hormone supports prostate development. Some studies show that older men have higher levels of DHT. Testosterone levels go down.
Procedures
Coming soon…
Treatments
Coming soon…
Urologic Cancer
Bladder Cancer
The bladder is a balloon-shaped organ in your pelvic area where your body stores urine before it leaves the body.
Bladder cancer is cancer that starts in the bladder. Non-muscle invasive bladder cancer is cancer that grows in the thin tissue on the inside surface of the bladder. This type of cancer has not spread into the bladder muscle or outside of the bladder. Muscle-invasive bladder cancer is a cancer that has spread into the muscle layer of the bladder wall. This is a more serious type of bladder cancer.
Causes
- Smoking cigarettes, cigars or pipes raises your risk of bladder cancer
- Long-term exposure to certain chemicals used to make plastics, paints, textiles, leather and rubber is also linked to a greater risk of bladder cancer
Symptoms
Possible signs of bladder cancer:
- Blood in the urine
- Frequent, urgent or painful urination
- Abdominal or back pain
Many of these symptoms often have less serious causes, but it’s important to have them checked by a doctor right away so the cause can be found and treated, if needed.
Procedures
Coming soon…
Treatments
Coming soon…
Prostate Cancer
What is Prostate Cancer?
What is the Prostate?
The prostate and seminal vesicles are part of the male reproductive system. The prostate is about the size of a walnut. The seminal vesicles are two smaller pairs of glands attached to the back of the prostate. The prostate sits below the bladder, in front of the rectum. It surrounds the urethra, a small tube that carries urine from the bladder out through the penis.
The main job of the prostate and seminal vesicles is to make fluid for semen. During ejaculation, sperm moves to the urethra. At the same time, fluid from the prostate and the seminal vesicles also moves into the urethra. This mixture— semen—goes through the urethra and out of the penis as ejaculates.
What is Prostate Cancer?
Cancer is the result of abnormal cell growth, which takes over the body’s normal cell function, making it harder for the body to work the way it should. Prostate cancer develops when abnormal cells form and grow in the prostate gland. Not all abnormal growths, also called tumors, are cancerous (malignant). Some tumors are not cancerous (benign).
- Benign growths, such as benign prostatic hyperplasia (BPH), are not life threatening. They do not spread to nearby tissue or other parts of the body. These growths can be removed and may grow back slowly (but often do not grow back).
- Cancerous growths, such as prostate cancer, can spread (metastasize) to nearby organs and tissues such as the bladder or rectum, or to other parts of the body. If the abnormal growth is removed, it can still grow back. Prostate cancer can be life threatening if it spreads far beyond the prostate (metastatic disease).
What is Early-stage Prostate Cancer?
Prostate cancer stays “localized” when cancer cells are found only in the prostate or even a little bit beyond it (extra-prostatic extension), but do not move to other parts of the body. If the cancer moves to other parts of the body, it is called “advanced” prostate cancer.
Prostate cancer is often grouped into four stages.
- Early-stage | Stages I & II: The tumor has not spread beyond the prostate. This is often called “early-stage” or “localized” prostate cancer.
- Locally Advanced | Stage III: Cancer has spread outside the prostate, but only to nearby tissues. This is often called “locally advanced prostate cancer.”
- Advanced | Stage IV: Cancer has spread outside the prostate to other parts such as the lymph nodes, bones, liver or lungs. This stage is often called “advanced prostate cancer.”
Symptoms
In its early stages, prostate cancer often has no symptoms. When symptoms do occur, they can be like those of an enlarged prostate or BPH. Prostate cancer can also cause symptoms unrelated to BPH. If you have urinary problems, talk with your healthcare provider about them.
Symptoms of prostate cancer can be:
- Dull pain in the lower pelvic area
- Frequent urinating
- Trouble urinating, pain, burning, or weak urine flow
- Blood in the urine (Hematuria)
- Painful ejaculation
- Pain in the lower back, hips or upper thighs
- Loss of appetite
- Loss of weight
- Bone pain
Updated August 2018
Causes
The cause of prostate cancer is unknown, but researchers know many things can increase a man’s risk for the disease.
- Age: As men age, their risk of getting prostate cancer goes up. Harm to the DNA (or genetic material) of prostate cells is more likely for men over the age of 55.
- Ethnicity: African American men have a higher rate of the disease. One in six African American men will be diagnosed with prostate cancer. Prostate cancer occurs less often in Asian American and Hispanic/Latino men than in non-Hispanic white men.
- Family History: Men who have a grandfather, father or brother with prostate cancer face a higher risk of getting the disease. Having family members with breast and ovarian cancer also raises a man’s risk for prostate cancer.
- Weight: Studies link being overweight in your 50s and later to a greater risk of advanced prostate cancer. Doctors advise keeping to a healthy weight to reduce risk.
What are the Signs of Prostate Cancer?
In its early stages, prostate cancer may have no symptoms. When symptoms do occur, they can be urinary symptoms like those of an enlarged prostate or Benign Prostatic Hyperplasia (BPH). Talk with your doctor if you have any of these symptoms:
- Dull pain in the lower pelvic zone
- Frequent need to pass urine
- Trouble passing urine, pain, burning or weak urine flow
- Blood in the urine (hematuria)
- Painful ejaculation
- Pain in the lower back, hips or upper thighs
- Loss of hunger
- Loss of weight
- Bone pain
Procedures
Coming soon…
Treatments
Coming soon…
Renal Cancer (Kidney Cancer)
What is Kidney Cancer?
Our kidneys’ main job is to filter our blood. Sometimes we develop masses (growths or tumors) inside our kidneys. Some of these growths are cancerous but many are not. You must have your mass checked out to learn if it is cancerous or not.
There are many different options for treatment. Often there are even more choices if your cancer is found early. Your medical team is there to help you. They can help you learn more about the pros and cons of treatments. Here we share more about kidney cancer and the steps you can take if a mass forms in your body.
What is the Purpose of our Kidneys?
Our kidneys serve many purposes, but they mainly do the following:
- Detoxify (clean) our blood
- Balance fluids
- Maintain electrolyte levels (e .g ., sodium, potassium, calcium, magnesium, acid)
- Remove waste (as urine)
- Make hormones that help keep our blood pressure stable, make red blood cells and keep our bones strong
What is a Kidney Mass?
A tumor, or mass, is an abnormal growth in the body. A kidney mass, or tumor, is an abnormal growth in the kidney. Some kidney masses are benign (not cancerous) and some are malignant (cancerous).
One in four kidney masses are benign. Smaller masses are more likely to be benign. Larger masses are more likely to be cancerous. Some tumors may grow slowly while some can be faster growing – or more aggressive. Aggressive tumors may form, grow and spread very quickly.
Most kidney growths (about 40%) are small, localized masses. Localized means that the tumor has not spread – from where it first started. The main classes of tumors are:
- Renal cell carcinomas (RCC). These are the most common malignant kidney tumors. They are found in main substance of the kidney, where the filtering occurs. RCC may form as a single tumor within a kidney or as two or more tumors in one kidney.
- Benign kidney tumors. About 20% of tumors removed from kidneys are benign. There are about nine named tumors in this class. Some can grow quite large but they are almost always non-cancerous and do not spread to other organs.
- Wilms tumors. Wilms tumors almost always occur in children and are rarely found in adults.
Basic Facts about Kidney Cancer
Kidney cancer is one of the top 10 most common cancers in the United States, with more than 76,000 new cases diagnosed each year. More men than women are diagnosed with kidney cancer. Kidney cancer can be seen in anyone but is more common in African Americans, American Indians and Alaskan Native people. You can get kidney cancer at any age but it is more common in older people (those greater than 75 years old). The earlier kidney cancer is diagnosed—the better your chances of survival.
What Causes Kidney Masses?
There is no known cause for developing a kidney mass. But there are a number of things that can increase your risk for kidney tumors such as:
- Smoking
- Obesity, poor diet
- High blood pressure
- Being on kidney dialysis
- Workplace exposure to chlorinated chemicals
- Heredity, which accounts for about 4-6% of kidney cancer cases
What are the Symptoms of a Kidney Mass?
Most kidney masses have no symptoms in the early stages. If there are symptoms, they will most likely be:
- Hematuria (blood in urine)
- Flank pain between the ribs and hips
- Low back pain on one side (not caused by injury) that does not go away
- Loss of appetite
- Weight loss not caused by dieting
- Fever that is not caused by an infection and does not go away
- Anemia (low red blood cell count)
Symptoms
Most kidney masses have no symptoms in the early stages. If there are symptoms, they will most likely be:
- Hematuria (blood in urine)
- Flank pain between the ribs and hips
- Low back pain on one side (not caused by injury) that does not go away
- Loss of appetite
- Weight loss not caused by dieting
- Fever that is not caused by an infection and does not go away
- Anemia (low red blood cell count)
Procedures
Coming soon…
Treatments
Coming soon…
Testicular Cancer
What is Testicular Cancer?
How Do Testicles Work?
The male reproductive organs include internal and external parts. The main reproductive organs are the penis, scrotum with testicles, and prostate.
These male organs are designed to:
- Make and release male sex hormones for growth of muscle, bone, and body hair
- Make and move sperm for reproduction, and fluid to protect it (semen)
- Carry sperm into the female reproductive tract
The testicles are two small egg-shaped glands, held in a sac below the penis (the scrotum). This is where sperm form and mature. From there, sperm moves into the vas deferens (a “tube” behind the testicles) and out the urethra when ejaculated. The testicles also make male hormones like testosterone. Testosterone controls the sex drive in men and starts the growth of muscle, bone and body hair.
Healthy testicles have a firm, slightly spongy feel. The firmness should be the same throughout. The size of both testicles should be about the same, though one may be larger than the other.
What is Testicular Cancer?
Testicular cancer happens when cells in the testicle grow to form a tumor. This is rare. More than 90 percent of testicular cancers begin in the germ cells, which produce sperm. There are two types of germ cell cancers (GCTs). Seminoma can grow slowly and respond very well to radiation and chemotherapy. Non-seminoma can grow more quickly and can be less responsive to those treatments. There are a few types of non-seminomas: choriocarcinoma, embryonal carcinoma, teratoma and yolk sac tumors.
There are also rare testicular cancers that don’t form in the germ cells. Leydig cell tumors form from the Leydig cells that produce testosterone. Sertoli cell tumors arise from the Sertoli cells that support normal sperm growth. Testicular tumors can be made of more than one type of cell.
The type of testicular cancer cell found, symptoms and other factors will help guide your treatment.
Procedures
Coming soon…
Treatments
Coming soon…
Pediatric Conditions
Benign (Not Cancerous) Uretheral Lesions Boys
What are Benign (Not Cancerous) Uretheral Lesions in Boys?
Irregularities of the urethra in young boys are rare. But they can cause problems with urination.
What Happens under Normal Conditions?
The urethra is a tube-like organ that carries urine from the bladder out of the body. In males, the urethra starts at the bladder and runs through the prostate gland, perineum (the space between the scrotum and the anus), and the entire penis. Normal urine flow is painless and can be controlled. The stream is strong and the urine is clear with no visible blood.
A lesion is a damaged part of an organ or tissue. The defect keeps the organ from working the way it should.
Types
There are a few different types of bengign uretheral lesions boys can develope. Your urologist will be able to determine which type of lesion your son has.
Urethral Polyps
A urethral polyp is a rare, irregular growth that most often appears at birth. It’s often made up of fibrous tissue. It may also include some smooth muscle, small cysts, or nerve tissue, all covered with a thin protective layer of tissue.
Meatal Stenosis
Meatal stenosis is when the hole at the penis tip is very small. This is caused by irritation around the hole. The irritation can lead to tissue growth and scarring across the hole. Meatal stenosis is most common in circumcised males, and seldom occurs in uncircumcised males. For more information on meatal stenosis please visit our comprehensive Urologic Conditons article.
Congenital Urethral Fistula
A urethral fistula is an abnormal passage (“fistula”) between the urethra and the outside of the penis. It’s called congenital when it occurs during growth before birth. The passage opens under the normal urethral hole at the end of the penis. During urination, two streams of urine may be seen. One will come from the urethral opening at the tip of the penis, and the other from the abnormal hole. The urologist often finds this condition by physical exam and watching the urination. This condition is rare.
Diverticulum of the Anterior Urethra
Diverticula are pouch-like enlargements of the lower urinary tract. They can happen in both the bladder and the urethra. Diverticula in the urethra make it wider.
This type of lesion can appear in 2 forms:
Saccular
This is the less severe condition. The diverticula rise from the floor of the urethra. This causes a weak urine stream, straining, and blocked urine flow. In some cases, the urethra can swell during urination.
Megalourethra
This is a more severe form, where the whole urethra is affected. There are 2 subsets of this condition:
Scaphoid megalourethra
This type of lesion happens when the spongy tissue (corpus spongiosum) around the urethra in the penis is missing.
Fusiform megalourethra
This lesion happens when both the corpus spongiosum and corpora cavernosa (the chambers that support the penis) are missing. In this case, the whole penis swells into a spindle-like form during urination.
The most common cause of urethral diverticulum is surgery that involves the urethra (such as for hypospadias). The urethra narrows downstream from the diverticulum. This raises the pressure in the urethra, causing the weak urethral tissue to balloon.
Cowper’s Duct Cyst
Cowper’s glands (also known as bulbourethral glands) are found under the prostate gland. These pea-sized glands make a clear, colorless fluid before ejaculation. This fluid cleans the urethra and neutralizes acid to protect sperm. It also provides a small amount of lubrication for sex. Cowper’s duct cysts occur due to abnormal narrowing at the opening into the urethra.
Urethral Duplication
Urethral duplication is a rare condition where a person is born with 2 urethras. It can be a complete copy of the organ with 1 or 2 openings, or just an extra urethra with a joined opening.
Symptoms
Symptoms of benign urethral lesions in boys depend on the type of lesion your son may have.
Urethral Polyps
If your son has a urethral polyp, there may be blood in his urine, signs of a urinary tract infection, or problems peeing. These can include:
- weak or broken urinary stream
- straining when peeing
- hesitating before urine flow starts
- stream stops suddenly
- dribbling at the end of urination
- painful urination
- a sense that the bladder hasn’t emptied
Meatal Stenosis
For more information on the symptoms of meatal stenosis please visit our information page on the condition.
Diverticulum of the Anterior Urethra
Some signs of urethral diverticulum are:
- urethra bulging during urination
- weak urinary stream with dribbling afterwards
- having urinary infections often
- other linked irregularities (such as prune belly syndrome)
Cowper’s Duct Cyst
Signs of a Cowper’s Duct cyst include:
- discomfort during urination
- bloody spotting
- a weakened urinary stream
- dribbling after urination
Urethral Duplication
While most cases of urethral duplication are found by chance, there are signs. Some signs are:
- 2 urinary streams
- infection in the extra urethra
- blocking problems from a buildup of material
Duplication often occurs as a blind ending that doesn’t get signals from the bladder. The duplicate urethra will almost always be on top of the normal urethra.
Procedures
Coming soon…
Treatments
Coming soon…
The physicians of the Wichita Urology Group are members of the American Urological Association and understand the importance of providing the most accurate and up-to-date information. This is why we have chosen to provide this content from the AUA’s Urology Care Foundation website.
